NR509 Week 1: Quiz
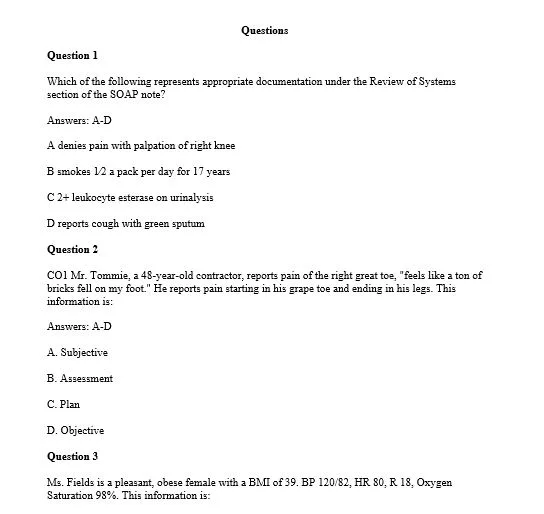
Question 1
Which of the following represents appropriate documentation under the Review of Systems section of the SOAP note?
Answers: A-D
A denies pain with palpation of right knee
B smokes 1⁄2 a pack per day for 17 years
C 2+ leukocyte esterase on urinalysis
D reports cough with green sputum
Question 2
CO1 Mr. Tommie, a 48-year-old contractor, reports pain of the right great toe, “feels like a ton of bricks fell on my foot.” He reports pain starting in his grape toe and ending in his legs. This information is:
Answers: A-D
A. Subjective
B. Assessment
C. Plan
D. Objective
Question 3
Ms. Fields is a pleasant, obese female with a BMI of 39. BP 120/82, HR 80, R 18, Oxygen Saturation 98%. This information is:
Answers: A-D
A subjective
B assessment
C plan
D objective
Question 4
A patient of American Indian descent presents to the clinic for a follow-up diabetic education session. During the health history interview, the nurse practitioner notices that the patient never makes eye contact and speaks mostly to the floor. This can be identified as using which of the following skilled interviewing techniques?
Answers: A-D
A active listening
B nonverbal communication
C summarization
D validation
Solution
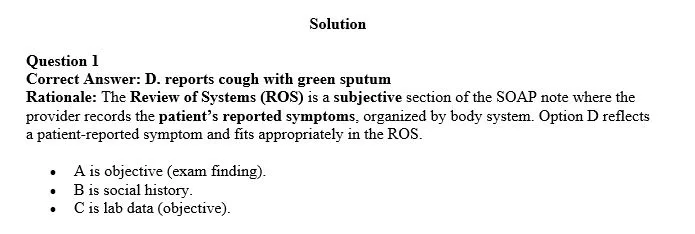
Question 1
Correct Answer: D. reports cough with green sputum
Rationale: The Review of Systems (ROS) is a subjective section of the SOAP note where the provider records the patient’s reported symptoms, organized by body system. Option D reflects a patient-reported symptom and fits appropriately in the ROS.
- A is objective (exam finding).
- B is social history.
- C is lab data (objective).
Download solutions to questions 1-4 for free
WhatsApp 0728626113 and we’ll work on the quiz for you
Reviews
There are no reviews yet.